- Startseite
- Forschung
- Arbeitsgruppen & Labore
- AG Corneal Stem Cell Biology
AG Corneal Stem Cell Biology
Research focus
The aim of this research group is to understand the mechanisms underlying the role of the limbal stem cells in corneal avascularity. Specifically, we are interested in the effect of UV irradiation on the limbal stem cell phenotype and pathological neovascularisation.
Introduction
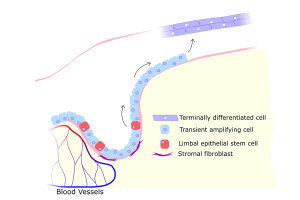
Vision is a key sensory function. Clear vision depends on transparency of the structures of the visual axis. Consequently, normal corneal tissue (the “windscreen of the eye”) is in an avascular and low inflammatory state. The limbal epithelial stem cells (LESC) maintain the integrity of the corneal epithelium thus preventing neovascularization, stromal scarring and conjunctivalisation (Figure 1.). These stem cells express the ATP binding cassette subfamily B member 5 (ABCB5), an ABC transporter and P-glycoprotein family member principally expressed in normal as well as cancerous stem cell populations. Although it has been proven both clinically and experimentally that LESCs destruction compromises corneal avascularity, the exact mechanisms by which this is achieved remain unidentified.
Our group focuses on elucidating these mechanisms and aims to identify new LESC-related regulators of corneal neovascularisation which will lead to new therapeutic options (we are part of FOR2240, “(Lymph)angiogenesis and cellular immunity in inflammatory diseases of the eye”). Exposure to UV irradiation compromises the LESC niche and induces corneal (lymph)angiogenesis. Pterygium, a non-cancerous tumour of the conjunctiva, is linked to UV-induced DNA and oxidative damage. The phenotype is associated with inflammation and neovascularisation causing discomfort and decrease of vision.
Preliminary evidence links pterygium onset to limbal epithelial stem cell (LESC) deficiency and own data suggest that following short term UV irradiation LESC become differentiated. However, a direct involvement of LESC DNA damage in the disease is not fully explored.
In addition, we are studying an ABCB5-expressing putative mesenchymal stem cell population in the human limbus which we believe is involved in the pterygium progression and its associated fibrosis.
Our hypothesis is that following UV insult, the inability of these stem cell populations to repair DNA damage contributes to induction of pterygia. In collaboration with the laboratory of Professor Björn Schumacher (CECAD) we investigate the possible links between UV damage and neovascularization.
Also, we explore the role of photolyase, a DNA repairing enzyme, as a therapeutic approach to prevent UV induced LESC damage leading to neovascularization, inflammation and thus pterygium.
Selected projects
The role of ABCB5 in corneal lymphangiogenesis
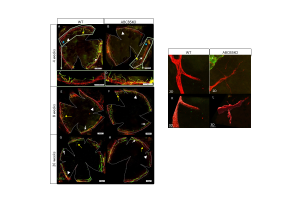
The limbus, the vascularized junction between the cornea and conjunctiva, is thought to function as a barrier against corneal neovascularization. However, the exact mechanisms regulating this remain unknown. In this study, the limbal epithelial stem cell (LESC) marker ABCB5 was used to investigate the role of LESCs in corneal neovascularization. In an ABCB5KO model, a mild but significant increase of limbal lymphatic and blood vascular network complexity was observed in developing mice (4 weeks) but not in adult mice (Figure 2.).
Conversely, when using a cornea suture model, the WT animals exhibited a mild but significant increase in the number of lymphatic vessel sprouts compared to the ABCB5KO, suggesting a contextual anti-lymphangiogenic effect of ABCB5 on the limbal vasculature during development, but a pro-lymphangiogenic effect under inflammatory challenge in adulthood. In addition, conditioned media from ABCB5-positive cultured human limbal epithelial cells (ABCB5+) stimulated human blood and lymphatic endothelial cell proliferation and migration. Finally, a proteomic analysis demonstrated ABCB5+ cells have a pro(lymph)angiogenic as well as an anti-inflammatory profile.
These data suggest a novel dual, context-dependent role of ABCB5+ LESCs, inhibiting developmental but promoting inflammatory (lymph)angiogenesis in adulthood and exerting anti-inflammatory effects. These findings are of high clinical relevance in relation to LESC therapy against blindness.
DNA damage in the limbal stem cell niche and implications on lypmphangiogenesis
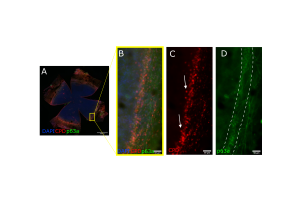
The cornea is frequently exposed to ultraviolet (UV) radiation and absorbs a portion of this radiation. UVB in particular is absorbed by the cornea and will principally damage the topmost layer of the cornea, the epithelium. Epidemiological research shows that the UV damage of DNA is a contributing factor to corneal diseases such as pterygium. There are two main DNA photolesions of UV: cyclobutane pyrimidine dimers (CPDs) and pyrimidine-pyrimidone (6-4) photoproducts (6-4PPs). Both involve the abnormal linking of adjacent pyrimide bases. In particular, CPD lesions, which account for the vast majority of UV-induced lesions, are inefficiently repaired by nucleotide excision repair (NER) and are thus mutagenic and linked to cancer development in humans. Here, we apply two exogenous enzymes: CPD photolyase (CPDPL) and T4 endonuclease V (T4N5). The efficacy of these enzymes was assayed by the proteomic and immunofluorescence measurements of UVB-induced CPDs before and after treatment.
The results showed that CPDs can be rapidly repaired by T4N5 in cell cultures. The usage of CPDPL and T4N5 in ex vivo eyes revealed that CPD lesions persist in the corneal limbus (Figure 3.). The proteomic analysis of the T4N5-treated cells shows increases in the components of the angiogenic and inflammatory systems. We conclude that T4N5 and CPDPL show great promise in the treatment of CPD lesions, but the complete clearance of CPDs from the limbus remains a challenge.
Key Publications
Meshko, B., et al… and Notara, M, ABCB5+ Limbal Epithelial Stem Cells Inhibit Developmental but Promote Inflammatory (Lymph) Angiogenesis While Preventing Corneal Inflammation. Cells, 2023.
Volatier, T., et al… and Notara, M, Short-Term UVB Irradiation Leads to Persistent DNA Damage in Limbal Epithelial Stem Cells, Partially Reversed by DNA Repairing Enzymes. Biology (Basel), 2023.
Clahsen, T., et al., The novel role of lymphatic vessels in the pathogenesis of ocular diseases. Prog Retin Eye Res, 2023.
Volatier, T., et al… and Notara, M, UV Protection in the Cornea: Failure and Rescue. Biology (Basel), 2022.
Domdey, M., et al… and Notara, M, Consecutive dosing of UVB irradiation induces loss of ABCB5 expression and activation of EMT and fibrosis proteins in limbal epithelial cells similar to pterygium epithelium. Stem Cell Res, 2022.
Notara, M., et al., Bevacizumab Induces Upregulation of Keratin 3 and VEGFA in Human Limbal Epithelial Cells in Vitro. J Clin Med, 2019.
Notara, M., et al., UV light-blocking contact lenses protect against short-term UVB-induced limbal stem cell niche damage and inflammation. Sci Rep, 2018.
Notara, M., et al., The Role of Limbal Epithelial Stem Cells in Regulating Corneal (Lymph)angiogenic Privilege and the Micromilieu of the Limbal Niche following UV Exposure. Stem Cells Int, 2018.
Notara, M., et al., Short-Term Ultraviolet A Irradiation Leads to Dysfunction of the Limbal Niche Cells and an Antilymphangiogenic and Anti-inflammatory Micromilieu. Invest Ophthalmol Vis Sci, 2016.
Notara, M., et al., Short-term uvb-irradiation leads to putative limbal stem cell damage and niche cell-mediated upregulation of macrophage recruiting cytokines. Stem Cell Res, 2015.
Collaborators
Prof. Dr. Bruce Ksander
- Massachusetts Eye & Ear Infirmary, Schepens Eye Research Institute, Boston, MA, USA
Prof. Dr. Markus Frank
- Transplant Research Program, Boston Children's Hospital, Boston, MA, USA
- Harvard Skin Disease Research Center, Department of Dermatology, Brigham and Women's Hospital, Boston, MA, USA
- Harvard Stem Cell Institute, Harvard University, Cambridge, MA, USA
- School of Medical and Health Sciences, Edith Cowan University, Perth, WA, Australia
Prof. Dr. Natasha Frank
- Harvard Stem Cell Institute, Harvard University, Cambridge, MA, USA
- Department of Medicine, VA Boston Healthcare System, Boston, MA, USA
- Division of Genetics, Brigham and Women's Hospital, Boston, MA, USA
Dr. Christoph Ganss
- TICEBA GmbH, Heidelberg, Germany
- RHEACELL GmbH & Co. KG, Heidelberg, Germany
Current funding
DFG, NO 1395/4-1
Project title: The role of ABCB5-expressing Pterygium Mesenchymal Stem Cells in Pterygium pathogenesis
Funding period: 02.2023-02.2026
Centre for Molecular Medicine Cologne, Career Advancement Program
Project title: Effects of UV irradiation on corneal angiogenic privilege: pterygium as a UV-induced stem cell disease model: The limbal niche and corneal avascularity
Funding period: 10.2018-12.2024
DFG, FOR 2240-2. TP N2
Project title: The role of ABCB5-expressing limbal epithelial stem cells in corneal lymphangiogenic privilege and pterygium pathogenesis
Funding period: 07.2018-06.2024